Nationwide Teleconsulting • Sports Nutrition E-Programs


Successful Nutrition Protocol for Gastrointestinal Issues in a Marathon Runner
 Exercise-induced gastrointestinal syndrome
Exercise-induced gastrointestinal syndrome
About 30 to 50% of endurance and up to 90% of ultra-endurance athletes experience some gastrointestinal distress during events such as a marathon, Ironman, or any long distance event that requires several hours of fuel and fluid replacement. One reason is that during hard exercise blood is moved away from our gut to the working muscles. Many of the symptoms athletes experience in training, but especially during races or events are similar to those experienced by persons with irritable bowel syndrome (IBS). Many of these athletes may even have been diagnosed with mild to moderate IBS-a condition which has been identified as inflammatory in nature.
What is a band-aide?
Sports nutritionists are trying to determine how to best help these athletes. Some recent suggestions have been to remove fermentable carbohydrates from the diet in the days leading to competition. However, this strikes me as a band aid as it does not address GI issues in training or address underlying inflammation. Removing these carbohydrates foods from the daily training season diet is not recommended as they provide valuable micronutrients, and fibers that produce beneficial prebiotics in the gut. The protocol to determine which fermentable carbohydrates cause an athlete distress is also very time consuming and not quickly personalized; there is a lot of trial and error involved. This approach focuses on intolerances, but what if the problem is really inflammation in the gut?
Do you want to guess at intolerances or address the real issue- inflammation?
Many GI symptoms are actually an indication of inflammation in the gut, as much of your immune system actually resides in your gut! As both a sports nutritionist and integrative/functional nutritionist, it is my clinical experience that addressing the inflammation is much more effective at reducing GI symptoms rather than guessing at intolerances. That’s because taking out foods that trigger inflammation (due to their immune response), calms the gut and allows for gut healing. Again, this results in better tolerance to food in the athlete, which in turn allows for better gut tolerance during exercise- both in training and events/competition.
Marathon runner with IBS
As an example, a 36-year old female runner came to me in May of 2018 in preparation for a Fall 2018 Marathon. She had been diagnosed with IBS (celiac was ruled out), and also complained of headaches, fatigue, and some skin issues such as rosy cheeks, itching, and flushing- also indicators of inflammation. Her goals were to identify food sensitivities, train without GI issues, develop a fueling plan for the marathon, decrease weight by 15 lbs, and of course race without any experiencing any GI distress.
Identifying food sensitivities early in the training season allows an athlete to undergo any food protocols before starting a heavier training cycle. She undertook the MRT test which is a clinically useful test for identifying hidden inflammatory responses to foods and food-chemicals. This MRT test identifies all non-IgE (allergy) food reactions involving multiple mediator-releasing pathways that can result in low-level sub-clinical inflammation or a symptom provoking inflammatory response. It is a personalized test rather than a one-size-fits-all protocol.
No symptoms after 14 days
Results of this test identified 32 of 170 tested foods and chemicals caused inflammation in this runner. I then created a personalized oligo-anti-inflammatory diet/group of foods for her based on her test results. For 14 days she consumed thirty-five low inflammatory foods providing carbohydrates, proteins, fats, and seasoning and avoided all added chemicals and other ingredients (not tested) often added in processing. By the end of day 14 on the protocol she reported having no symptoms whatsoever- no GI issue in daily life or while running, no headaches and improved energy. Via the LEAP protocol designed for the maximum benefit from the MRT test, she continued to add back low inflammatory foods while monitoring her reaction it to any of these foods.
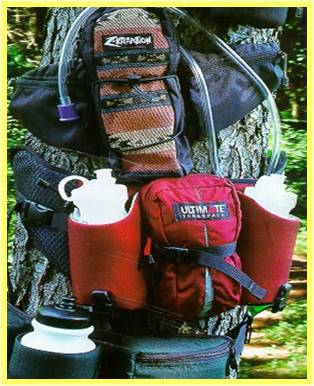
After 60 days on the protocol, she was consuming a wide variety of foods and timing macronutrients properly for long runs, speed work, and optimal recovery. Her weight trended down until she had lost 15 lbs in 16 weeks, a rate of weight loss that did not compromise her training and recovery. A fueling plan utilizing sports drinks and gels that were not derived from inflammatory ingredients was developed. She was instructed on checking her sweat rate and fueling with 60 g of carbohydrate every hour. Her performance in the long runs improved with better refueling and hydration practices. She continued to experience no GI problems during these runs and successfully completed the marathon. She continues to avoid reactive foods, but has a wide variety of foods that she can consume daily for a well-balanced training diet.
Professional assistance is available!
Endurance athletes with GI concerns can benefit greatly from identifying inflammatory foods and following a personal anti-inflammatory diet during training. This also provides a framework for developing a race fueling plan that can be practiced in training, well in advance of competition.
Personal Nutrition Designs, LLC offers comprehensive sports nutrition services for marathon and triathlon competitors as well as comprehensive lab testing that supports athletes in decreasing inflammation and improving micronutrient status.