Nationwide Teleconsulting • Sports Nutrition E-Programs


Wellness Blog
Vitamin D and your immunity
May 19, 2020
 Vitamin D – An underlying condition and a public health failure
Vitamin D – An underlying condition and a public health failure
By Monique Ryan, MS, RDN, LDN
Why is Vitamin D so important for your immune system?
We have been aware of the importance of vitamin D for the role this vitamin hormone plays in many aspects of our health for over a decade, including optimizing and strengthening our immune system. Vitamin D, unlike other vitamins, is a hormone used by the body to signal genes that affect immune function. This vitamin hormone also helps our immune system’s T –cells function properly. Vitamin D also plays a role in the regulating and suppressing the inflammatory “cytokine storm” that likely causes the acute respiratory distress seen in severe COVID-19 cases.
Vitamin D and Covid-19
In late April, the first data on COVID-19 and vitamin D from 3 hospitals in southern Asia measured vitamin D status (blood levels) and severity of symptoms. They found that 86-percent of all cases among patients with normal vitamin D levels were mild. Conversely 73-percent of cases among patients with vitamin D deficiency were severe or critical. So lower vitamin D levels were associated with more severe coronavirus symptom and high vitamin D levels were associated with less severe symptoms.
Researchers from Northwestern University analyzed patient data from 10 countries including China, France, Germany, Italy, Iran, South Korea, Spain, Switzerland, the UK and US. Countries with high mortality rates such as Italy, Spain, and the UK had lower vitamin D levels compared to patients in countries not as severely affected. The team at Northwestern also discovered a strong correlation between low vitamin D levels and the risk of high inflammation called the cytokine storm. A cytokine storms is a condition that can severely damage lungs and lead to the acute respiratory distress syndrome that seems to kill the majority of COVID-19 patients.
In a study published in the Irish Medical Journal researchers also analyzed the vitamin D levels among adult populations in Europe and compared these with COVID-19 infection and death rates. Adults living in the sunny countries of Spain and Italy actually had lower vitamin D levels and higher rates of true vitamin D deficiency, as well as the highest death rates in Europe. More northern countries of Norway, Finland, and Sweden had higher vitamin D levels, lower rates of deficiency, despite less sunlight exposure. However this was due to the more common practice of vitamin D food fortification and vitamin D supplementation in these countries.
Rates of COVID-10 infection and death rates have been much lower in Norway, Sweden, and Finland compared to Italy, Spain, and several other European countries. Researchers concluded, “the correlation between low vitamin D and deaths from COVID-19 is statistically significant.” In addition, they advised that the Irish government recommend that all adults take vitamin D during the coronavirus pandemic to treat deficiency. The same researchers also pointed out that age, diabetes, hypertension, and being in a nursing home all raise the risk of vitamin D deficiency.
Another group of researchers from the US and Hungary recommended that people at higher risk for infection from COVID-19 and other viral infections raise their vitamin D blood concentrations to 40-60 ng/dl. Currently conventional medical advice is to raise the level above 32 ng/dl, though many experts have called for the 40-60 ng/dl level as well.
Vitamin D levels in the US
Recent data from Grassroots Health indicated that over 50-percent of Americans are vitamin D deficient and insufficient. Levels were higher in minorities with over 75% of Blacks and Hispanics vitamin D deficient/insufficient. In the United States 60-percent of nursing home residents were found to be vitamin D deficient. COVID-19 data suggest a disproportionate burden of illness and death among racial and ethnic minority groups, and among nursing home residents.
Clearly we need to do more in regards to vitamin D status, particularly for at risk individuals who are currently at risk and to offer immune support. It is best to get vitamin D levels tested to determine the degree of supplementation required for each individual.
Vitamin D and Diet
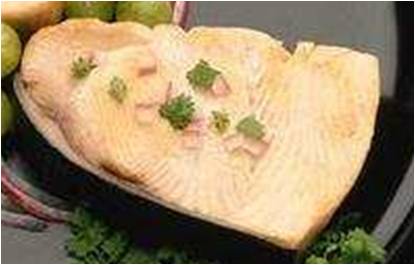
Diet remains a poor way to obtain vitamin D. Short of eating a pound of wild-caught salmon daily (about 2000 IU) or other fatty fish, very few foods naturally provide vitamin D. Some items like milk, some yogurts, cereal, and orange juice, and non-dairy milks are fortified with about 100 IU.
Sunlight exposure produces vitamin D, but from October to May anyone living north of Atlanta, Georgia does not receive adequate sun exposure. Sun exposure should be for 10 to 15 minutes at high noon several time weekly for lighter skinned persons. Longer exposure times are required for darker skinned persons. Sunscreen, recommended by dermatologists for any sun exposure, blocks vitamin D production.
The Institute of Medicine has set the Recommended Dietary Allowance (RDA) of vitamin D at 600 international units (IU) for everyone under the age of 70. (It’s 800 IU for adults 70+.) However many experts believe that is too low. The Tolerable Upper Limit is 4,000 IU, meaning that dose could be safely taken daily.
Many physicians and nutritionists routinely put their patients on 1000 to 2000 IU daily. Others may need higher doses to maintain optimal blood levels. For persons that are severely deficient, very high doses may be needed and only taken under a physician’s supervision. One a deficiency is corrected, a lower maintenance dose can be taken. Blood levels can be monitored and retested to ensure find what is the best amount for an individual.
Clearly we need to do more regarding the vitamin D status of many Americans, and now more than ever.